
Reports have emerged in which physicians express a diminished enthusiasm for their profession, noting that administrative tasks were less about patient relationships and more about coding, billing, reimbursement, and compliance.

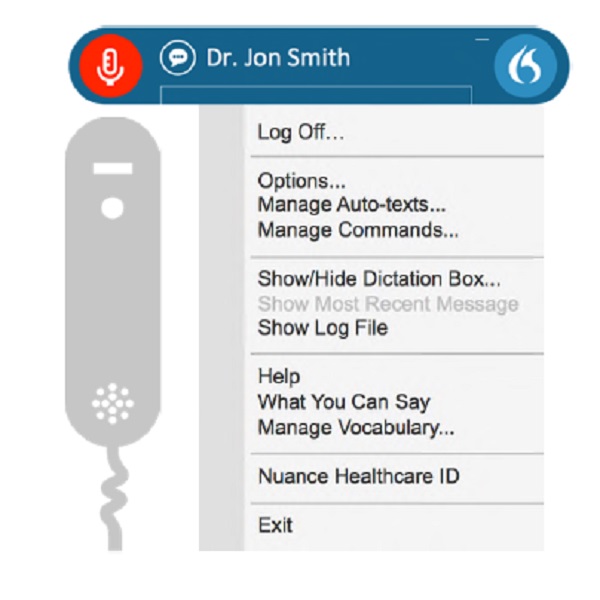
The medical transcription industry is starting to see an uptick in dictation volumes as health care providers begin to realize the woes of generating documentation themselves. The situation is exacerbated by the transition to bundled and value-based payments. Health care providers need a means to document more details about the patient narrative than those represented in EMR templates, drop-down lists, and check boxes. There’s little doubt that clinical documentation has become more complex. Health care providers continue to express frustration with completing these clinical documentation tasks which are often undertaken with the patient sitting in front of them, a time when they should be focusing on capturing the patient’s story in detail so that they can refer to these notes with confidence and share the information with other health care professionals. Front-end speech recognition requires providers to edit/proofread their results to ensure the templated information was entered correctly and dictated text was accurately recognized.
#Dragon medical 360 price how to
Health care providers are expected to spend considerable hours learning the integrated features of an EMR which may include any or all of the previously mentioned templates, drop-down lists, and seemingly endless screens of check boxes, as well as learn how to properly dictate. To make clinical documentation easier for the health care providers, the EMR industry has produced cookie-cutter templates, drop-down lists, and check boxes. This staggering figure illustrates the criticality of accurate clinical documentation for health care quality, patient safety, and accurate coding and billing. Recently, Health and Human Services announced it had collected a record-breaking $28.7 million in HIPAA settlements last year. As part of the negotiation with the transcription vendor, the provider will demand lower line rates and tighter turnaround times. If these organizations have in-house transcription, they will look to transition those employees to other positions within the organization or potentially partner with a transcription vendor. In turn, there will be a plea to physicians and hospital caregivers to self-document. The project is targeted to take around 18 months.Īs facilities and organizations pursue these types of expensive projects, there will be a push for cost savings. In a recent Becker’s Health IT & CIO Report, it was reported that Buffalo, New York-based Catholic Health is investing more than $100 million in a project to implement an Epic EHR. Let’s first start by looking at the cost of EHR implementations.

In fact, many have wondered, is it dead yet? A Victim of Cost Cutting
As a result, there is a perception that medical transcription, as part of revenue cycle management, is a dying occupation. Nevertheless, health care providers will continue to seek cost-saving measures by eliminating in-house medical transcription and contracting with transcription services. While the Department of Labor does predict a 3% decline from 2016 through 2026, the numbers support the fact that the profession is still viable and that there will continue to be a demand for medical transcription health care services such as medical tests and procedures grow. According to the Bureau of Labor Statistics, in 2016 there were approximately 57,400 medical transcriptionists or health care documentation specialists in the United States.


 0 kommentar(er)
0 kommentar(er)
